Cataract surgery has evolved into a highly sophisticated and precise field within ophthalmology. Our ability to have such successful outcomes hinges on good diagnostic measurements and accurate intraocular lens (IOL) power calculations.
As ophthalmology residents embark on their journey to becoming skilled surgeons, understanding the intricacies of IOL power calculation becomes paramount.1
This comprehensive guide aims to provide residents with an in-depth exploration of why proper calculation is critical, relevant terms, the breakdown of biometry, calculation formulas, clinical pearls, and a thoughtful conclusion to solidify key takeaways.
Significance of accurate IOL power calculation
The importance of accurate IOL power calculation cannot be overstated in the realm of cataract surgery. Accurate IOL power calculation extends beyond refractive precision; influencing factors such as the patient's independence, safety, and satisfaction.
It serves as the linchpin for achieving optimal visual outcomes and patient satisfaction. A miscalculation can lead to
post-operative refractive errors, impacting the patient's vision and overall quality of life.
Therefore, residents must appreciate the gravity of this step in the surgical process and recognize its direct correlation to patient well-being. For residents, mastering IOL power calculation is not just a technical skill but a journey toward enhancing the overall patient experience. Making sure that all calculations are double- or even triple-checked for accuracy is vital before each surgery.
Key components for IOL calculations
- Axial Length (AL): The distance from the corneal epithelial surface to the retinal pigment epithelium, axial length is a critical parameter influencing the refractive power of the eye. Accurate measurement is crucial for precise IOL power calculation.2
- Corneal Power (K Value): Measured in diopters, corneal power represents the curvature radius of the cornea. It significantly influences the eye's overall refractive power and is a key parameter for calculating IOL power.
- Anterior Chamber Depth: This parameter denotes the distance between the cornea and the iris. Understanding anterior chamber depth is essential for selecting the appropriate IOL, as it contributes to the overall optical system of the eye.
Other notable measurements include lens thickness, white-to-white distance, estimated lens position, and corneal thickness. However, these measurements play less of a critical role for calculations. White-to-white measurements become particularly important when an anterior chamber IOL (ACIOL) or an
implantable collamer lens (ICL) will be planned for use.
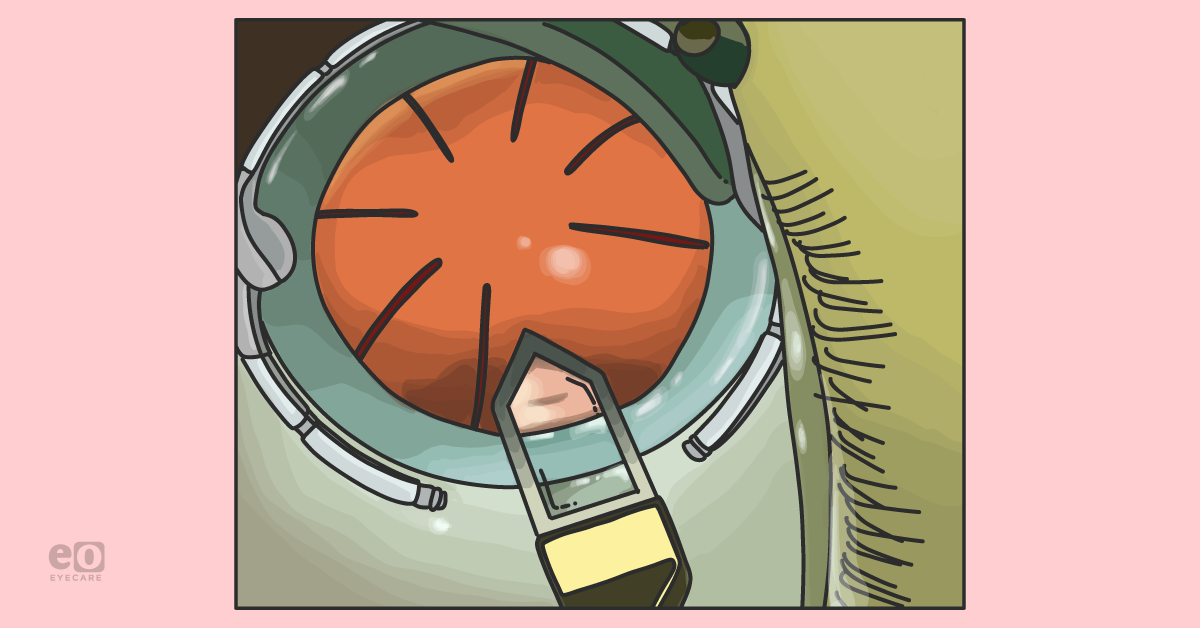
Breakdown of biometry in IOL power calculations
Biometry—the ability to measure all these key components—plays a pivotal role in accurate IOL power calculation.
Residents should master and understand the importance of the following steps in biometry:
- Axial Length Measurement: Utilizing techniques such as optical coherence biometry or ultrasound, surgeons can measure the axial length accurately. The choice of method may depend on factors like patient characteristics (dense cataract) and surgeon preference.
- Knowing how to interpret these values is pivotal. Some surgeons would repeat measurements for any outcomes that differ by greater than 0.2mm between the eyes to ensure accurate measurements were taken.
- Corneal Power Measurement: Using keratometry or corneal topography, residents measure the curvature of the cornea in diopters. This measurement is crucial for input into various IOL power calculation formulas.
- It is important to note that certain ocular surface conditions, such as dry eye and anterior basement membrane dystrophy (ABMD), can affect these measurements—therefore, they should be adequately treated pre-operatively (and before biometry is performed for surgery).
- Corneal power is also very critical when planning to treat astigmatism during cataract surgery. Understanding when you have good measurements is important because you want to ensure you have the ability to correct as much refractive error for each patient as possible.
- Anterior Chamber Depth Measurement: Employing optical or ultrasound methods, surgeons measure the distance between the cornea and the iris. Precise measurement of anterior chamber depth is essential for selecting the most suitable IOL.
Clinical pearls for IOL power calculations
To enhance the accuracy of IOL power calculation and refine their skills, residents should learn the following clinical pearls:
1. Optimize biometry techniques
Precision in biometry techniques is paramount. You need to be able to rely on your results. Residents should continuously refine their skills to minimize variability in measurements and ensure consistent accuracy.
The more you practice, the more you understand when your results look like outliers. Current biometers used in practice then to be more accurate and have a greater capacity to measure through dense cataracts. In training, the use of contact or immersion A-scan may be used for calculations.3
2. Validate equipment calibration
Regular calibration of biometric devices is essential. Ensuring that equipment is accurately calibrated contributes to reliable measurements and, subsequently, precise IOL power calculations. Residents should take the opportunity to learn how to calibrate instruments because, after training, there may not be anyone who can do it accurately.
3. Consider patient factors
Patient-specific characteristics, such as a history of
refractive surgeries or eye trauma, should be factored into the IOL power calculation. Adapting the approach based on individual patient profiles contributes to improved outcomes.
4. Surgeon's A-constant
Fine-tuning the A-constant (A-constants are used directly in Sanders-Retzlaff-Kraff [SRK] II and SRK Theoretical (SRK/T) formulas. The constant is a theoretical value that relates the lens power to AL and keratometry, it is not expressed in units and is specific to the design of the IOL and its intended location and orientation within the eye.
Based on personal experience and outcomes is a crucial aspect of IOL power calculation. Regular review and adjustment of the A-constant enhance the predictability of post-operative refractive outcomes. This is a critical and advanced step in cataract surgery outcomes, however, every surgeon should be working to optimize their A-constant by consistently
tracking all of our patient outcomes after surgery.
4Established formulas for IOL calculation
Residents must gain proficiency in understanding and applying the right IOL power calculation formulas. It is also imperative to understand the history and evolution of these formulas to understand the different key components related to formula accuracy. Various formulas cater to specific patient characteristics, ensuring a personalized approach to cataract surgery.
Some of the earlier used formulas include:
- SRK/T Formula: This was developed from the older version of the SRK II formula. This formula has been a workhorse for many years and remains widely used. It incorporates axial length, corneal power, and anterior chamber depth, providing a straightforward and effective method for IOL power calculation.
- IOL Power = A-constant + 2.5(Axial Length) - 0.9(K Value)
- Hoffer-Q Formula: Developed as an alternative to SRK/T, the Hoffer Q formula is particularly useful in eyes with long or short axial lengths. It incorporates additional factors, including age, to refine the calculation.
- IOL Power = A-constant + 2.5(Axial Length) - 0.9(K Value) + 0.1(Age)
- Haigis Formula: This formula is recognized for its accuracy, especially in eyes with long axial lengths. It incorporates additional parameters such as the lens thickness and the anterior chamber depth, offering a more comprehensive approach to IOL power calculation. The a, b, and c are IOL constants used in this formula.
- IOL Power = A-constant + Spherical Equivalent – a(Axial Length) + b(K Value) + c
In addition to these popular established IOL formulas mentioned above, several other established and widely used formulas are essential for ophthalmologists and residents to be familiar with. Each formula has its strengths and limitations, and the choice of formula often depends on the patient's characteristics and the surgeon's experience.
Here are some important IOL formulas:
- Holladay I Formula: The Holladay I formula is known for its versatility and is often used in eyes with long or short axial lengths. It considers axial length, corneal power, anterior chamber depth, and the effective lens position.
- Barrett Universal Formula: Developed by Graham D. Barrett, MD, this formula aims to improve the predictability of IOL power calculation across a range of eye conditions. It considers axial length, corneal power, and anterior chamber depth.
- SRK II Formula (Sanders, Retzlaff, and Kraff II): This uses a fixed A-constant and may be employed in eyes with average axial length.
- OptiSpheric Intraocular Lens Calculation (Olsen Formula): The Olsen formula considers axial length, corneal power, and anterior chamber depth, aiming to improve accuracy in IOL power calculation, particularly in eyes with long axial lengths.
- Theoretical/T Formula: Similar to SRK/T, this formula is a theoretical approach that uses a fixed A-constant and is suitable for eyes with average axial length.
- Fyodorov IOL Formula: Developed by Svyatoslav Fyodorov, MD, this formula is known for its simplicity and is suitable for eyes with axial lengths within the average range.
- Thomson Formula: This formula incorporates axial length and corneal power, providing an alternative method for IOL power calculation.
It's important for ophthalmologists and residents to recognize that no single formula is universally applicable to all cases. The choice of formula should be tailored to the individual patient, considering factors such as axial length, corneal power, anterior chamber depth, and the surgeon's experience.
Newer generation formulas for IOL calculation
With the advent of newer generation formulas and advancements in technology continuing to shape the landscape of IOL power calculation, many surgeons are opting to ditch some of these older formulas to use the so-called “newer generation formulas,” emphasizing the need for ongoing learning and adaptation in the field of ophthalmology.
Here are some of the newer generation IOL formulas that are more widely used today:
- Barrett Universal II (BUII) Formula: Building upon the success of the Barrett Universal Formula, the BUII takes into account additional factors, such as the estimated lens position (ELP), and is designed to provide improved outcomes in various eye conditions. This formula has been shown to be effective in short and long eyes.
- Hill-RBF (Radial Basis Function) Formula: This formula employs machine learning techniques to enhance the predictability of IOL power calculation. By incorporating a large dataset of patient outcomes, it aims to optimize accuracy across a broad range of ocular parameters.
- Kane Formula: Developed by Jack Kane, MD, this formula integrates advanced mathematical modeling to improve the accuracy of IOL power calculation, particularly in eyes with previous refractive surgery.
- Pentacam AXL Formula: Utilizing data obtained from Pentacam (a topography/tomography device) measurements, this formula enhances the accuracy of IOL power calculation by incorporating anterior chamber depth, keratometry, and lens thickness.
- EVO Formula: The EVO formula combines historical biometric data with artificial intelligence to optimize IOL power calculation. It adapts to a surgeon's individual outcomes and aims to improve refractive accuracy.
- Olsen Formula: This formula is designed to provide better outcomes in eyes with long axial lengths. It incorporates various parameters such as axial length, corneal power, anterior chamber depth, and lens thickness.
- Barrett True-K Formula: This formula is an enhancement of the Barrett Universal Formula and is designed to improve accuracy in eyes with irregular corneas. It takes into account the true net power of the cornea, which may be particularly relevant in post-refractive surgery eyes.5
- Camellin-Calossi Formula: Developed for eyes with previous myopic laser refractive surgery, this formula aims to improve IOL power calculation in situations where traditional formulas may be less accurate.
I recommend all surgeons—especially residents—get comfortable using a combination of formulas, review the predicted outcomes, and then follow up with the actual outcomes. This way, each surgeon can gain a personalized understanding of each formula’s accuracy.
IOL power considerations for toric IOLs and post-refractive surgery patients
It is important to note that the choice of formula may not just depend on the specific characteristics of the patient, but also their expected surgical outcomes if they opt to proceed with advanced technology IOLs, such as
toric IOLs, or if they are post-refractive surgery patients.
Post-refractive surgery patients create a unique challenge that can cause a refractive surprise after cataract surgery if not designated correctly. There is a level of estimation with all biometers used that can incorrectly calculate a lens power for cataract surgery if it is not noted that the patient has had previous refractive surgery.
In addition, whether the patients have had prior hyperopic or myopic
laser-assisted in situ keratomileusis (LASIK)/photorefractive keratectomy (PRK) or radial keratotomy (RK) matters as well. For these specific scenarios, there are formulas and considerations that aim to address the unique challenges associated with astigmatism and altered corneal surfaces.
In both toric and post-refractive cases, it's crucial for ophthalmologists to carefully select the appropriate formula based on the individual patient's history, the nature of the refractive procedure, and the desired visual outcome.
Additionally, advanced diagnostic technologies, such as corneal topography and
optical coherence tomography (OCT), can provide valuable information to enhance the accuracy of IOL power calculations in these challenging cases. Regular updates and familiarity with the latest research in the field are essential for staying informed about the evolving landscape of IOL power calculation in toric and post-refractive patients.
Here are some important IOL formulas and considerations for toric and post-refractive patients:
Toric IOL formulas
- Barrett Toric Calculator: This is an extension of the Barrett Universal Formula and is specifically designed for toric IOLs. It incorporates additional parameters related to astigmatism correction, such as the axis of astigmatism.
- Holladay Toric Calculator: An adaptation of the Holladay I formula, the Holladay Toric Calculator is used for toric IOL power calculations. It considers factors like the astigmatic axis and the surgically-induced astigmatism (SIA).
- Koch Astigmatic Factor: Often used in conjunction with other formulas, the Koch astigmatic factor is applied to adjust the spherical equivalent and astigmatism in toric IOL power calculations.
Post-refractive surgery IOL formulas
- Double-K Method: This method involves using both pre-operative and post-operative keratometry readings to calculate IOL power. It is particularly useful in eyes that have undergone corneal refractive procedures, such as LASIK or PRK.
- Haigis-L Formula: An adaptation of the Haigis formula, the Haigis-L includes an adjustment for eyes that have undergone corneal refractive surgery. It considers the corneal power change induced by the surgery.
- Shammas-PL Formula: Developed by H. John Shammas, MD, this formula is designed for IOL power calculation in eyes with previous myopic or hyperopic LASIK or PRK. It considers the corneal power change induced by refractive surgery.
- Masket Formula: The Masket formula is specifically developed for eyes that have undergone myopic LASIK. It incorporates factors such as the pre-operative keratometry and the amount of refractive change induced by the surgery.
- Savini Formula: This formula is designed for IOL power calculation after corneal refractive surgery. It considers the surgically induced change in corneal power and anterior chamber depth.
- Fechtner Formula: Developed for eyes with prior RK, the Fechtner formula aims to provide accurate IOL power calculations in these cases.
- Effective Keratometry Readings (EKR) Formula: This approach involves calculating the effective keratometry readings by taking into account the changes in corneal power induced by refractive surgery.
Final thoughts
As the field of ophthalmology continues to advance, newer formulas will continue to spring up and refinements to existing ones may emerge. Accurate IOL power calculation is not merely a technicality but a cornerstone of successful cataract surgery.
For
ophthalmology residents, it represents a critical skill to be honed and mastered. This journey involves understanding the significance of accurate calculation, familiarizing oneself with key terms, mastering biometry techniques, and applying appropriate calculation formulas.
In conclusion, residents should approach IOL power calculation as a dynamic and evolving skill that requires continuous learning and adaptation. By prioritizing precision, considering patient-specific factors, and staying abreast of advancements in technology and surgical techniques, residents can contribute significantly to the field of ophthalmology.
Ultimately, the goal is to provide patients undergoing cataract surgery with the best possible visual outcomes, ensuring a clearer and brighter future for all.