It is not uncommon in history for major medical breakthroughs to be discovered by “accident” or as an unforeseen outcome of scientific study.
It was said that Chinese soldiers were the first to stumble upon a form of rudimentary
orthokeratology.
1 They would sleep with sandbags over their eyes overnight, and upon waking, they had improved distance vision.
Then, in 1962, George Jessen described a technique called "orthofocus" where he was able to manipulate a refractive change in the cornea of up to -1.00.2 Not unlike orthokeratology, red light therapy has been around in China for multiple decades.
However, it was not initially intended for myopia control but instead for amblyopia treatment. Practitioners discovered that red light therapy not only improved
amblyopia but also slowed axial length progression.
Although there is very little published data, one study by
Malik et al. reported that red light filters, compared to neutral density filters/no filters, resulted in a reduction of axial length and refractive error.
3What is the proposed mechanism behind RLRL therapy?
Since the growing popularity of repeated low-level red light (RLRL) in the past decade for
myopia control, many researchers have been trying to understand the mechanism behind this treatment. RLRL therapy results do not match with classical emmetropization theory in that red light, which is a long wavelength, would focus behind the retina and therefore induce axial elongation.
One explanation for this was introduced by
Gawne et al., who proposed a theory that under red light irradiation, the long-wavelength opsin was over-activated and the short-wavelength opsin was underactivated. This signaled the eye to develop in the direction of hyperopia to compensate for the imbalance of short- versus long-wavelength activation.
4Furthermore, studies have shown that red light may provide a protective effect on the retinal tissue. It was found in one study that red-light enhanced mitochondrial function and increased the survival rate of cells.5 In support of this finding, red light therapy has been shown in both animal and clinical studies to reduce oxidative stress and inflammation which may be involved in regulatory pathways of myopia.6,7
Many studies examining red light therapy for myopia control have found an increased choroidal thickness (discussed later). The choroid has been found to play a crucial role in relaying signals from the retina to the sclera. Many scientists believe that alteration of the synthesis of scleral extracellular matrix results in changes to ocular size and therefore axial length.8,9
How is RLRL therapy administered?
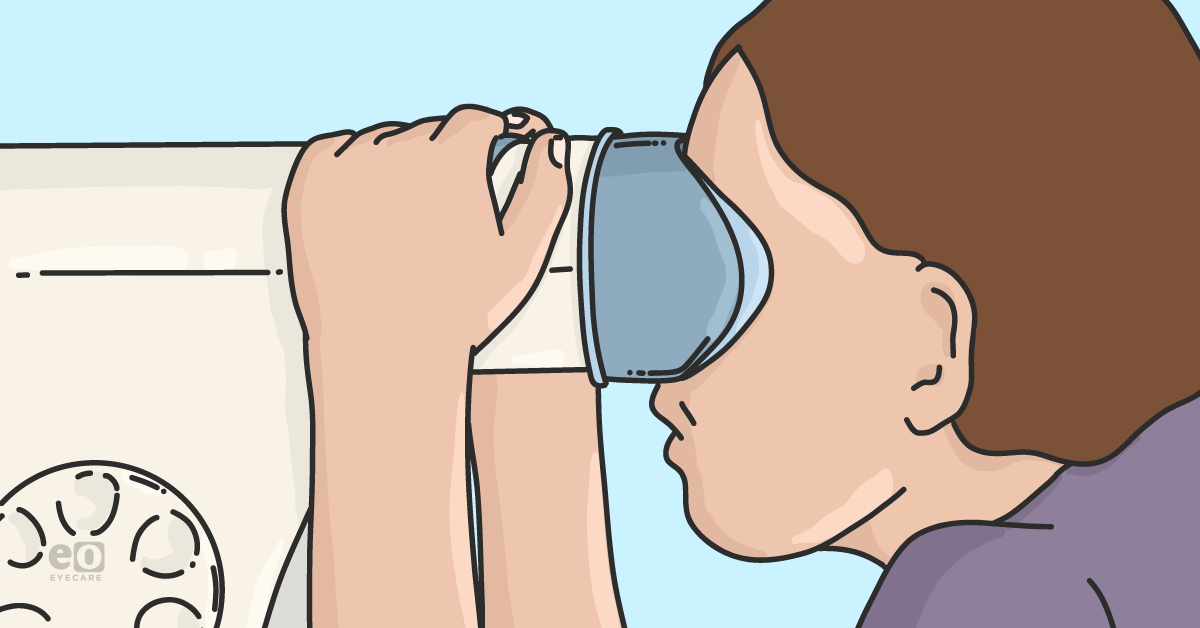
As of now, the only instrument currently used for RLRL therapy is the
Eyerising device which is approved in Australia, New Zealand, the United Kingdom, the European Union, and China. This device emits 650nm using 2.0+/-0.5mW and is used twice a day for 3 minutes, 5 days a week.
The patient wears normal distance glasses during treatment. All the major studies discussed today use this instrument and protocol. Here is a
link to better understand the treatment procedure with the Eyerising.
Has RLRL therapy been proven to slow myopia?
A study by
Jiang et al. followed 264 children ages 8 to 13 with refractive errors from -1 to -5D for 12 months. Not only did they find that the RLRL therapy group showed a significant mean reduction in axial length (0.26mm) and refractive error (0.59D) between the RLRL and control group, respectively, but that RLRL therapy was able to achieve >0.05mm axial length
shortening in 39.8% of participants at 1 month and 21.6% participants at 12 months.
10How could the axial length possibly be shortened? Well, the authors also measured the choroidal thickness and found it to increase on average by 16.1μm at the 1-month visit. However, not all of the axial shortening (-0.04mm) changes can be explained solely by choroidal changes (16.1μm) due to a discrepancy in the size of the change. It was postulated that scleral collagen remodeling or increased blood flow was responsible for the leftover shortening in axial length.10
Another study by
Wang et al. confirmed that RLRL can result in axial length shortening. Their subjects ranged from 3 to 17 years old and were followed for 12 months. They found that 26.5% had 0.05mm/year shortening, 17.51% had 0.10mm/year shortening, and 4.61% had 0.20mm/year shortening over the 12-month period.
11Furthermore, the authors discovered a significant increase in the frequency of axial length shortening with increasing baseline age, axial length, and refractive power. In other words, children with higher
myopia and younger age demonstrated greater axial length shortening. Therefore, perhaps this type of treatment modality may be beneficial for younger patients and/or higher myopia (>-5.00D).
11Can it prevent the onset of myopia?
One study by
He et al. followed pre-myopic children with refractive errors ranging from -0.50 to +0.50D. They sought to investigate whether RLRL therapy could reduce the incidence of myopia, not just slow it. Results showed a 54% reduction in the incidence of myopia within a 12-month period.
12Furthermore, they found better efficacy in both refractive error and axial length slowing for subjects starting between +0.01 to +0.50D baseline than -0.50 to 0.00D baseline. These findings support the belief that RLRL is beneficial for pre-myopic children.12
Is there a rebound effect after RLRL therapy?
All the studies previously mentioned have demonstrated success with RLRL therapy. However, these results were based only on a 12-month time span. Additionally, they did not investigate what happened once RLRL therapy was discontinued.
Therefore,
Xiong et al. (2022) studied children ages 8 to 13 with refractive error of -1 to -5D. They split up the children into four groups: SVS-SVS, SVS-RLRL, RLRL-SVS, and RLRL-RLRL. At the 12-month mark, subjects either stayed in their initial modality or switched to the opposite treatment.
13The main group of interest was the RLRL-SVS group to see if the effects of RLRL were maintained after switching to single vision spectacles (SVS). In fact, they did find a significant rebound effect. The authors tried to potentially justify the rebound effect due to the age of the children (on average 11 years old) which are still expected to show significant eye changes.13
A study by
Smith et al. supported this rebound effect after they found that tree shrews who were initially receiving RLRL therapy recovered from induced hyperopia and went back to normal emmetropization once treatment was discontinued.
14How does RLRL therapy compare to other myopia control modalities?
So the question remains, how does RLRL treatment compare to the efficacy of orthokeratology and atropine?
Xiong et al. (2021) studied children ages 6 to 16 with refractive error >-0.50D who were either assigned to the orthokeratology, RLRL, or the control group and followed for 6 months.
15Axial length and choroidal thickness were measured and compared among the three groups. RLRL showed the greatest efficacy with axial length shortening (-0.06mm), while ortho-k came in second (0.06mm) with a reduction but not shortening of axial length.
The control group showed axial elongation (0.23mm). Furthermore, the mean subfoveal choroidal thickness change was greatest in the RLRL therapy group (14.98μm) after 6 months, followed by ortho-k (35.3μm). The control group actually showed choroidal thinning (-16.84μm).
On the surface, the study demonstrates superior efficacy with RLRL, however, we must remember that this study was only 6 months long and therefore not enough data to provide strong support for one treatment over the other.15
A study by
Chen et al. compared atropine 0.01% to RLRL. They enrolled children 7 to 15 years old with >-1.00D refractive error and followed for 12 months. Subjects were either assigned to the RLRL group or the atropine group. There was no control group.
16Results did not show an overall shortening of axial length in the RLRL group. However, the RLRL group demonstrated a significant slowing of axial length compared to the atropine group (0.08mm vs. 0.33mm, respectively).16 There was a brief period of axial length shortening in the first 3 months of this study which matches with Xiong et al.'s findings (discussed above).
However, remember that Xiong et al.’s study was only 6 months long and may have shown overall axial length elongation after a longer period of time. This shows the importance of long-term trials to understand the full picture of treatment efficacy.
Are there any reported adverse events with RLRL therapy?
There is currently only one case study by
Liu et al., who reported a 12-year-old female with bilateral vision loss for 2 weeks after 5 months of RLRL therapy.
17 The patient complained of abnormally bright lights and prolonged after-images after RLRL treatment sessions. The
optical coherence tomography (OCT) images before RLRL therapy were normal for both eyes.
Post-treatment OCT scans demonstrated foveal ellipsoid disruption and interdigitation zone continuity. Multifocal
electroretinogram (ERG) revealed moderate and mild decreased response in the macular and paramacular regions, respectively. After 3 months without RLRL therapy, bilateral outer retinal damage partially recovered, and visual acuity (VA) improved to 20/25 OU.
17Is it safe to use this device?
A
new study was released in 2024 investigating the safety profile of RLRL devices (i.e., the
Sky-n1201a and Future Vision) similar to the RLRL therapy devices (i.e., Eyerising) used in the studies mentioned earlier in this article.
18 All of the RLRL devices are Class 1 lasers.
Class 1 lasers are considered low-powered devices that are safe when viewed accidentally and briefly, such as a laser printer.
The authors discovered that both devices, which required 3-minute sessions of continuous exposure, surpassed the maximum permissible exposure (MPE) and, therefore, could result in photochemical damage. Only the Sky-n1201a had a risk of thermal damage unless the pupil was smaller than 4.25mm in diameter. The Future Vision device had no risk of thermal damage.
The American National Standards Institute (ANSI) has developed
safety requirements for ophthalmic equipment exposing direct optical radiation into/at the eye. ANSI recommends that, after reaching the MPE, the same intensity of light should not be viewed for at least
48 hours.
In the current study protocols, subjects are required to use the device for 3 minutes twice a day. Therefore, researchers and doctors are warned to be careful when using RLRL therapy at its current protocol since it may lead to long-term retinal damage.18
In conclusion
RLRL therapy is emerging as a promising new
treatment modality for myopia control. Multi-year studies will need to be conducted to investigate the long-term efficacy of RLRL therapy and the potential rebound effects once discontinued.
Currently, RLRL is working to gain FDA approval so it may be available in the US in the near future. As a doctor, it is important to understand the benefits and risks before starting a myopia control treatment and
monitor your patients closely for any adverse events.